However healthy you are when you decide to relocate, you’ll eventually need medical care. And whether at home or abroad, you’ll probably need more as the years go by — so learn all you can about a country’s healthcare delivery and requirements before you make the move.…
Janice MacDonald, Ex-Pat Life Isn’t Always Easy
I did do my homework before deciding to have my hip replaced in the Netherlands.
I read everything I could find about the procedure and recovery, consulted experts in my network, and even watched first-hand experiences on YouTube. Medicare was always my fallback: surgeons in the U.S. were just as skilled, and similar techniques are used on both sides of the Atlantic. But one key difference stood out—the follow-up care. In the U.S., post-op guidance seemed to be little more than a handout of home exercises, whereas the Netherlands provided two full weeks of residential physiotherapy. That level of support made my decision easy. Chris and I set the dates, arranged transport from Annadal operatiecentrum to the Plataan revalidatiecentrum, booking Chris a hotel next door for my two-week stay. As a bonus, I even hit Platinum status with Delta by confirming the hotel stays.
Naively, I thought that all of the contingencies were settled and I was good to go.
When things took an unexpected turn two months later, every plan went out the window. I found myself alone, facing emergency surgery in an unfamiliar hospital, while Chris was a day away in the UK, unable to get to me immediately. “Two weeks and you’ll be out,” they assured me. But by the time I was finally discharged, four months had passed. The experience was nothing like what I had planned, but it taught me many lessons about navigating healthcare abroad, confronting my own aging, and the strength of steadfast relationships.
- The plan is more of a guideline. When the incision didn’t close and the lab values failed to normalise, the instructions changed day by day. Try to walk as much as possible. Stay in bed on your back and don’t leave the room. Adaptive, committee-based reviews became the norm. The specialists were excellent, but they needed to abandon fixed protocols in order to respond to events. From my perspective, certainties were measured in days: there was no lasting plan for what came next. Where I tried to draw a line for myself, If it came to a revision, I would ask them to patch me up so that I could fly to the US, was not actually an option.
- Other patients are the benchmarks. I got along well with all of my roommates and fellow patients throughout. Some spoke some English (generally the younger), others not at all. We wished each other well on surgery days, traded lab results and observations, kept track of the criteria for discharge. Some were lost souls, crying for family or tumbling into my bed during confused night wanders. Most kept constructively cheerful: sharing about family, pets, and plans for home.
- The food is Dutch. I never adjusted to the native sequence or substance of the meals. Bread, processed meats, and cheese for breakfast and dinner; potatoes, overcooked meats and very steamed vegetable for lunch. I found my way into coffee, fruit, muesli, and yogurt (eventually hard-boiled eggs) for the start and end of the day, the more recognisable main for lunch. Vitala+ offered wine and pie in the cafe, and evening treat; the hospital’s ‘Bel en Bestel’ service brough cornflakes and gehaktballen. And they did make a real effort at Christmas: Venison, wine, golden eggs and decorated cookies.
- Brexit is a curse. In early November, when they decided that 10 more weeks of surgery and recovery were needed, we realised that Chris’ leave to remain was expiring. The rule is 90 days out of 180, no compassionate exceptions. She would have to leave until February. Together with family in the US, principally my mom and brother, we all adapted to a WhatsApp simulacrum of being present: Text messages, photos, video calls. Not at all easy or satisfying, but a lifeline throughout.
- Holidays are hardest. Thanksgiving was the worst: it’s not a Dutch celebration and it’s hard to explain how much I missed that. They did a lot for Christmas: visiting pianists and choirs, a collection of wandering shepherds and wise men on Christmas Eve, lots of midnight noise at New Years. They decorated everywhere nicely: It wasn’t the Magische Market at the Vrijthof or Expat Turkey Dinner in London though. As such, it was less of a comfort than it was a reminder of what I was missing.
- Staying steadfast through repeated recovery. Each surgery was a milestone: I would wake from anesthesia checking for any loss of movement, numbness, or cognitive dysfunction. I was light-headed from the blood loss; the incisions seemed to get wider and deeper with each round. But it was mostly the climb back each of five times: first just standing, then a few steps. Able to reach the bathroom with a frame, a roller, finally just a crutch. Accommodating IVs / PICCs, their tubes and pumps, alarms for cartridge changes every couple of hours all night. I needed to build strength and cardiovascular tone though, avoid bone and muscle atrophy while giving the next group of surgeons a good canvas to work on. The close availability of the weight and fitness machines was great: I could spend over two hours every day on hand bicycling, hand weights, and leg lifts. My determination became a bit of a joke to residents and staff alike, and I came out looking more fit than when I went in (jokingly called it all ‘A trip to holiday camp’).
- Personalising the routine. The experience is very institutional: Lights on at 0730, off at 2100. Four-times daily checks of temperature, pulse, pain, poo. The house staff around at 0930; the specialists weekly. I fit exercise around the 0800-1230-1730 meal times, retreated to the cafe for a glass of wine nd some study each evening. I haunted the ‘quiet room’ set up to calm stress – a TV with idealised winter scenes and flickering electric candles. I became a devotee of the Vendee Globe, an around the world solo sailboat race, with updates each morning from SailWorld.com. I followed a couple of amiable travel vloggers solo adventuring in Asia (Sabbatical Tommy from New York and Ryan Palmer from New Zealand). I took up two studies: DataCamp for Machine Learning and a Pandas Programming book (both of which are good mental exercise and sleep inducers). A diverse smattering of Nederlands workbooks was attempted, none of which helped in keeping up with my lunch table’s conversations. I read fiction books and essay collections again, helping me to avoid the Presidential news and the compelling doom-loops of Instagram, YouTube, and TikTok.
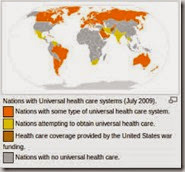
- The Dutch care system works well. The quality of staff, nursing, aides, PTs, and facilities maintenance was outstanding. Most spoke English, all were relentlessly upbeat and endlessly patient. My Dutch insurance company (VGZ) never questioned the care decisions, I never got a bill beyond the deductibles, and my November renewals went through without a big increase. Set against the horror stories out of UnitedHealthcare in the US, I wonder what could have happened had I run into the same circumstances under Medicare. The UK-NHS could have been worse yet: my local experiences in England have been a struggle to gain GP access, specialist referrals, and effective (or even palliative) treatments.
- Dont be alone; never fall. I’d expected most patients to be post-surgical, stroke follow-up, or trauma rehabilitation. In fact, the majority had falls at home, and were kicking themselves for not being more careful. Many had laid, undiscovered, for hours before a neighbor found them because they lived alone. Both factors delayed them being able to return home, and seemed to me like the most significant aspect of elder care that needs re-consideration. Many of the 90+ year olds with me were clear-eyed, social, could tell a good story, and dove into the group PT and games-over-coffee activities each day. But, like me, they couldn’t be discharged until they could be independent: that meant strong enough to be independent (I had a 40-stair goal) and able to live within available support nearby family, neighbors, home health care visits).
- There’s no place like home. Stoicism can help in the face of changing circumstances, but a discharge date is the event that I most looked forward to. Discharge meant seeing Chris again (I was determined that I would walk to greet her without any aids), enjoying a coffee out along the winter streets, sleeping in late and making breakfast, choosing food from a store shelf or restaurant menu, driving to do errands, making plans for a trip. Ordinary normalcy. I worried about the transition out after being regimented, alone, contained, supported for so many months. It turns out not to have been an issue: my life picks up and goes on. I’m different in my head about health care delivery, the Dutch, aging, and making the most of retirement than when I went in. But I appreciate the ordinary things regained through lots of people’s efforts and support after many, many months away.
‘reflecting on the whole experience, I replied to Janice just after Christmas, 2024:

Well observed Janice. I’ve lived in the Netherlands for 16 years and recently, at 70, needed to rely on the local health system for 6 months when my hip implant became infected. It has made me reflect on expat health care., with three thoughts to add: 1) Do as much as you can to stay healthy and out of the health system for as long as possible. Pay attention to basics: diet, exercise, sleep, stress, regular preventative care, staying connected. 2) Keep good coverage that will pay for inpatient and supplemental care when you need it. Good insurance costs a fraction of what it does in the US and expat policies easily patch gaps. 3) Decide where you have confidence in doctors and facilities – once you are in hospital care you can’t board a plane to change countries. I chose a hernia repair in the US Medicare and a hip replacement in the NL, and am happy with both choices. But both were a commitment to see it through to the finish in that system, no matter what.



 I’m never too certain of dentists outside the United States, so always save my dental checkups for visits back across the pond. It leaves me with longer between appointments than I would like, and no backups if there is a tooth emergency, but my comforts is much higher.
I’m never too certain of dentists outside the United States, so always save my dental checkups for visits back across the pond. It leaves me with longer between appointments than I would like, and no backups if there is a tooth emergency, but my comforts is much higher. I explained why I discounted the result, why I disliked the Omron, and that my blood pressure was normally a healthy 110/70.
I explained why I discounted the result, why I disliked the Omron, and that my blood pressure was normally a healthy 110/70. The doctor listened to my story, then ran a right and left arm clinical measurement with a cuff and stethoscope. She listened to my heart and my carotids. She thumped my chest a couple of times. Then, sShe made notes and smiled: ‘You’re healthier than I am, honestly.’
The doctor listened to my story, then ran a right and left arm clinical measurement with a cuff and stethoscope. She listened to my heart and my carotids. She thumped my chest a couple of times. Then, sShe made notes and smiled: ‘You’re healthier than I am, honestly.’